Skin Cancer Treatment
Skin cancer can arise from many factors, including sun exposure. We treat a large variety of skin cancers, but most commonly basal and squamous cell carcinomas and melanoma. Below is some basic information about the various types of skin cancer and treatment options. For additional information about skin cancer treatments, please contact us to schedule a consultation.
Melanoma is the most serious skin cancer and requires the most aggressive treatment. Dr. Economou treats melanoma arising in any part of the body and is the only Twin Cities Plastic Surgeon performing sentinel lymph node biopsy for staging of the disease. He works closely with other specialists who care for melanoma patients to ensure that treatment and outcomes are optimized.
Most patients have suspicious lesions first examined and biopsied by their primary care physician or dermatologist. Once the diagnosis is established, a treatment plan is initiated. Whether or not radiation or chemotherapy is needed will be determined by the final pathology report.
Cutaneous melanoma is amongst the most aggressive forms of skin cancer. It originates in the pigment cells of the skin (melanocytes) at the junction of the epidermis (upper skin layer) and dermis (thicker, deeper skin layer). Its’ incidence is rising steadily and the lifetime risk in the U.S. is now approximately 1 in 50. About 30 % of melanoma arise in a pre-existing mole and 70% in otherwise normal skin. There are many factors which increase one’s risk of developing melanoma. These include:
- Skin type—fair skinned people of Northern European ancestry have higher risk
- Family history of melanoma—especially in a parent/sibling
- Personal history of melanoma – raises risk for developing another melanoma unrelated to the first
- Ultraviolet ray exposure – can be sunlight or through tanning booth; blistering sunburns significantly raise the risk of later melanomas
- Number of moles – people with many moles have higher risk
- Personal or family history of dysplastic (precancerous) moles
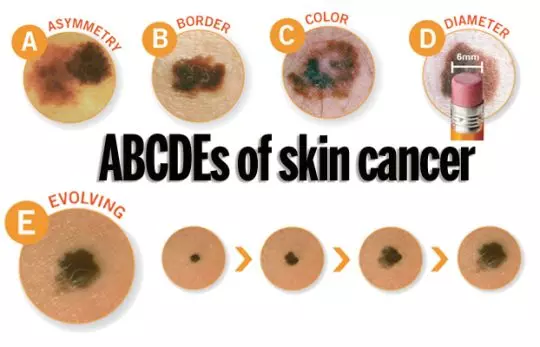
The clinical signs of a melanoma lesion are best remembered by the ABCDE rule.
A: asymmetry in the shape of the mole
B: border irregularity in the edges of the mole
C: color is irregular and can be many shades of brown/black/red/white
D: diameter greater than the size of the tip of a pencil eraser (6mm)
E: enlarging size of mole over time
Source: American Academy of DermatologyIf you develop a mole with any of these features, you should be examined by a dermatologist.
Lesions suspicious for melanoma will be biopsied using a variety of techniques. This is not done to treat the melanoma, but establishes the diagnosis so that further treatment can be appropriately planned.
The pathology report on the biopsied lesion will contain a great deal of information regarding the skin cancer that then allows the surgeon to appropriately treat the tumor. The primary factor in determining prognosis and treatment is the depth of invasion. This is a measurement representing the distance the melanoma cells have invaded into the skin. Deeper melanomas have more contact with blood and lymphatics vessels and are associated with a higher risk of spread. In addition, melanoma can exhibit very specific features under the microscopic exam that, if present, indicate potential aggressive behavior raising the risk of spread. These include ulceration (erosion of the skin), regression (scar/inflammation around tumor indicating immune system reaction), elevated mitotic rate (a measure of tumor growth), lymphovascular invasion (tumor directly invading blood or lymphatic vessels), perineural invasion (tumor growth into small nerves of skin) and satellite lesions (separate areas of tumor surrounding the primary site). The presence of any of these features would prompt more aggressive surgical treatment of the melanoma.
At your initial consultation, a general discussion about melanoma will occur and the specific features of the newly diagnosed melanoma reviewed. Surgical treatment of the melanoma will also be discussed. How a melanoma is treated is determined by the demonstrated depth and features present. In general, superficial melanomas (<0.75 mm) without aggressive features are treated with wide excision only. This is usually done under local (injected) anesthesia at a minor procedure area at Abbott Northwestern Hospital in Minneapolis. Melanomas require wide excision to minimize the risk of recurrence. The width of the margin of skin removed is determined by the depth of the tumor. For non-invasive melanomas, a margin of 5 mm is needed. Melanomas invasive up to 1 mm deep require a 1 cm margin circumferentially. Melanomas between 1-2 mm deep require a 1-2 cm margin and any melanoma of 2mm or more depth requires a 2cm margin be taken. All excisions are done to the level of the muscle. Excisions are usually done in an elliptical (football) shape, which lengthens the scar, but contours it so it will better blend with the surrounding skin. This means the resultant length of the scar will be approximately 2 1/2 to 3 times the diameter of the excised area.
Depending on the area affected, closure of the surgical defect will be done with primary approximation, local tissue rearrangement or a skin graft. Your surgeon will discuss the details of wound care and healing.
In addition to wide excision, Sentinel Lymph Node biopsy is done to rule out microscopic spread of tumor to regional lymph nodes. Early spread is often undetectable by radiologic scans or physical exam and is best diagnosed by lymph node biopsy. Lymph nodes are grouped in clusters that serve specific regions. Arms and legs are served by nodes in the axillae and groin respectively. The trunk is also served by the axillary/groin nodes. The head/neck region is served by lymph nodes in the neck area. Physical exam of the nodes is done to rule out enlarged or hardened nodes. Even in the absence of physical abnormality, microscopic spread is not ruled out. The status of the Sentinel Lymph Node is then used to complete staging of the tumor and guide further treatment.
National standards are used to determine the need for Sentinel Node Biopsy based on risk. Typical criteria indicating need for lymph node biopsy are:
- Tumors of over 0.75mm or Clark Level IV depth
- Ulcerated tumors or tumors with aggressive features on microscopic exam
- Tumors with a mitotic index of over 1/square mm
- Tumors with indeterminate depth
Patients with deep tumors (>4mm) often require a preoperative CT scan to rule out distant metastasis. If evidence of distant metastatic disease were identified on a scan, the patient would be referred to a Medical Oncologist before surgery.
Wide excision and Sentinel Lymph Node Biopsy are done at the same time under a general anesthetic as an outpatient at Abbott Northwestern Hospital. On the day of surgery, the exact node connected to the site of the melanoma and its location is determined 2 hours before surgery with a Lymphoscintogram.
This is a Nuclear Medicine study and involves injection of a small amount of a low level radioactive tracer around the original biopsy site. Within an hour, it travels to the lymph node connected with that site following the same path as the tumor would take. That node then becomes radioactive and lights up under x-ray. This does not mean that there has been spread to the lymph node. It is a map guiding removal of the proper node. During surgery, a blue dye is injected into the skin that will stain the node blue. That gives the surgeon two separate markers to look for at surgery to ensure the proper node is removed. This dye is excreted in the urine and turns it blue for a day or two. The skin around the excision site may also have a blue hue for a short time. This will resolve on its own.
Pathology takes 2-3 working days to complete. The final report will reflect examination of both the skin and lymph node. The status of the node determines the final stage and need for further treatment. If the node is benign, no further treatment is needed. Nodes with metastatic disease require consideration of further treatment. A PET/CT scan of the body would be ordered in patients with metastasis in the Sentinel Lymph Node to rule out disease elsewhere. In addition, consultations would be arranged with a Medical Oncologist to discuss immunotherapy and with a Surgical Oncologist to discuss possible complete removal of the lymph nodes in the area of the Sentinel Node.
Melanoma is divided into four stages (plus sub-stages) indicating how far the tumor has advanced.
- Stage 0: noninvasive melanoma (melanoma in situ)
- Stage 1a: superficial melanoma (<o.75 mm) without ulceration
- Stage 1b: melanoma 0.75-2mm deep with no ulceration and benign sentinel lymph node
- Stage IIa: melanoma 1-2 mm deep with ulceration and benign sentinel lymph node OR 2-4 mm deep with no ulceration and benign sentinel lymph node
- Stage IIb: melanoma 2-4 mm deep with ulceration and benign sentinel lymph node OR >4
- mm deep with no ulceration and benign sentinel lymph node
- Stage IIc: melanoma >4 mm deep with ulceration and benign sentinel lymph node
- Stage III: melanoma of any depth with satellite tumor or metastasis to sentinel lymph node
- Stage IV: melanoma of any depth with metastasis to distant organs/structures
Routine surveillance for melanoma patients in stages 0 to IIa includes Dermatologist total body skin exams every 3 months for 1-2 years with physical exam of the lymph nodes and thorough yearly physical exams.
Patients with stage IIb disease or higher need the above surveillance plus regular visits with a Medical Oncologist.
Stage III & IV patients are candidates for immunotherapy. This is not chemotherapy, but drugs that enhance the immune system’s ability to fight cancer better. Most patients can tolerate this therapy and lead a normal life during treatment. In addition, regular radiologic scans are done to rule out recurrence. Stage III patients will also be referred to a Surgical Oncologist to discuss the possibility of complete surgical removal of all lymph nodes from the area of the sentinel lymph node. This is done if more extensive disease is present in the lymph node removed. Radiation therapy is occasionally used in very specific situations and patients are referred to a Radiation Oncologist if needed.
Your surgeon will review the above information with you in detail at your initial consultation and discuss with you the details of your biopsy and surgical plan. Melanoma is a serious condition; the keys in maximizing survival are appropriate treatment and surveillance. We are committed to treating your melanoma quickly and are always available to address any questions or concerns you may have. We only work with other medical specialists who are experts in their field (particularly in melanoma care) and will arrange any additional consultations/referrals as needed.